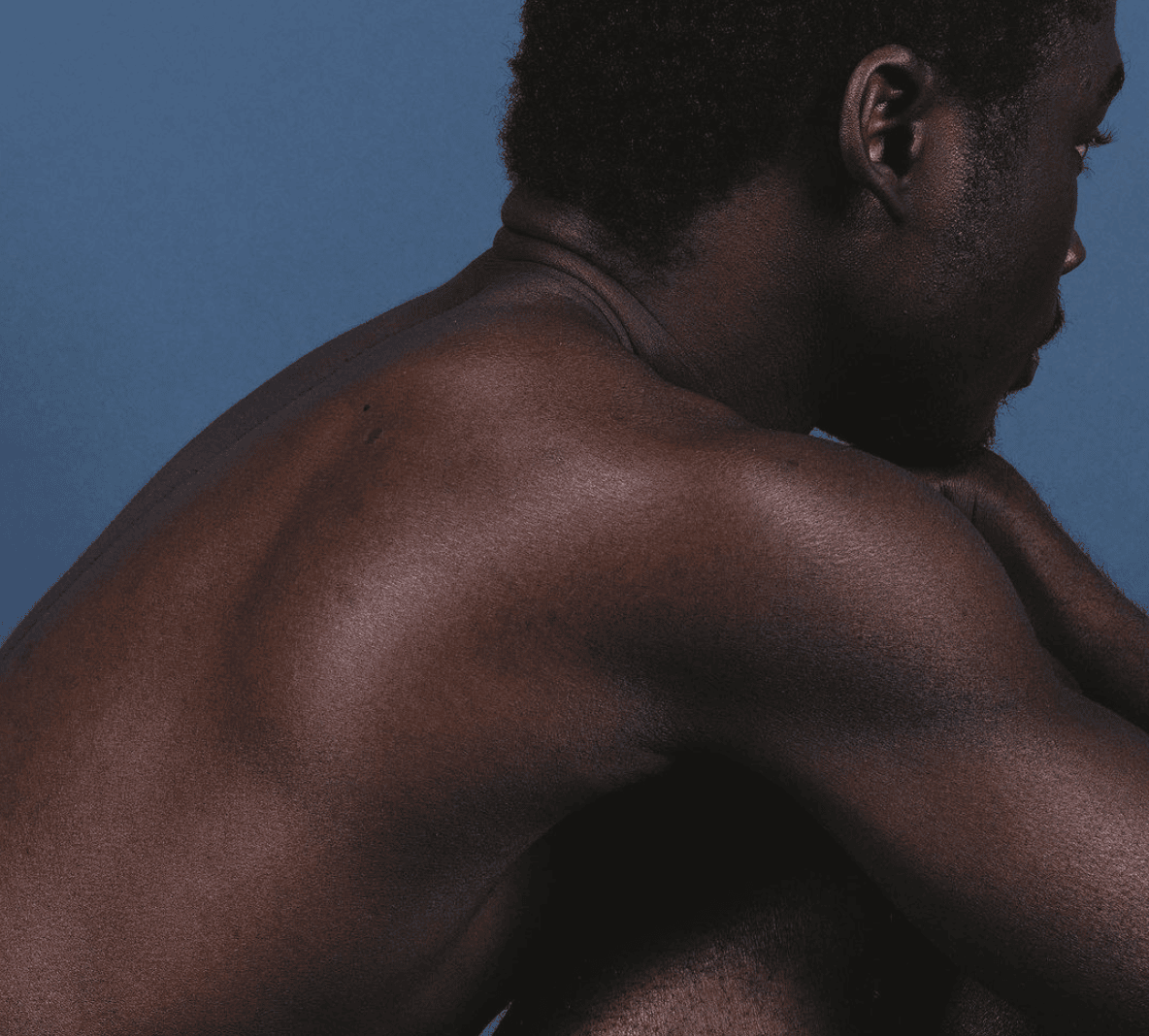
Men’s Mental Health: Awareness and Suicide Prevention
Men’s mental health is too often ignored — yet it is fundamental to overall wellbeing.
Across the United States, many men quietly struggle with symptoms of anxiety, depression, or emotional exhaustion, while feeling pressure to stay composed and self-reliant. Cultural expectations around masculinity can make it difficult to express vulnerability or seek professional help — leaving many to cope in silence.
To change this, we need to understand the unique obstacles men face — from stigma and social conditioning to biological and emotional dynamics. This article explores the most common mental health challenges among men, the contributing factors, and the steps that can support resilience and lasting wellbeing.
By normalizing open conversation and ensuring access to compassionate, evidence-based care, we can shift the narrative of strength and support healthier emotional lives for men everywhere.
The State of Men’s Mental Health in the U.S.
Prevalence and the Treatment Gap
Mental illnesses are common in the United States. In 2022, about 23.1 % of adults experienced some form of mental illness (National Institute of Mental Health, 2023). Yet, men’s mental health conditions often go undetected or untreated. Research shows that men are significantly less likely to seek care, and many receive treatment only after their symptoms have severely worsened (Journal of Men’s Health, 2023).
Men die by suicide roughly four times more often than women, despite being diagnosed with depression less frequently (Association of American Medical Colleges [AAMC], 2023). This discrepancy highlights a hidden crisis — many men suffer without access to or utilization of support.
A systematic review on stigma found that men’s reluctance to seek help is strongly linked to the internalization of masculine norms throughout their lives (Pederson & Vogel, 2021).
These findings reveal a troubling truth: emotional suffering among men often goes unnoticed until it becomes critical.
What Drives Mental Health Strain in Men?
Men’s mental health challenges arise from a complex interplay of biological, social, and cultural factors.
Biological and Genetic Influences
While men and women share many biological risk factors, emerging research suggests that sex-specific hormonal responses and stress regulation may shape how mental health symptoms manifest (Smith et al., 2024).
However, large-scale studies disaggregating biological differences in mental health remain limited, leaving many questions open for future research (Journal of Men’s Health, 2023).
Social Determinants and Life Stressors
Men often face pressures tied to their societal roles: job demands, economic instability, relationship strain, and social isolation. Major life transitions — such as unemployment or divorce — can precipitate depressive episodes (Affleck et al., 2023). Additionally, structural factors such as poverty or discrimination further widen disparities in mental health outcomes (Thompson et al., 2024).
Masculinity Norms, Stigma, and Help-Seeking Barriers
One of the most potent obstacles is the internalization of traditional masculine norms — emotional suppression, and self-reliance — that make vulnerability feel unsafe (Mokhwelepa & Sumbane, 2024). Men who strongly adhere to these beliefs are significantly less likely to talk about emotional distress or seek mental health care (Seidler et al., 2016).
Self-stigma, or viewing one’s own distress as weakness, amplifies these challenges (Pederson & Vogel, 2021). Clinicians may also overlook male-typical symptoms such as irritability, aggression, or substance use, mislabeling them as behavioral issues rather than expressions of depression or anxiety (Cochran & Rabinowitz, 2020).
Coping Strategies and Substance Use
Men are more likely to adopt externalizing coping behaviors — such as alcohol use, risk-taking, or aggression — to manage emotional pain (Möller-Leimkühler, 2023). These behaviors often mask underlying depression or anxiety, delaying recognition and treatment.
Common Mental Health Conditions in Men
Men are affected by a broad spectrum of mental health disorders, though their symptoms and patterns of expression often differ from women’s.
1. Depression and Mood Disorders
Men may underreport sadness or hopelessness, resulting in underdiagnosis. Instead, depression in men may appear as irritability, anger, or risk-taking behavior (Seidler et al., 2016). This contributes to fewer diagnoses and greater suicide risk.
2. Anxiety Disorders
While anxiety disorders are often diagnosed more frequently in women, many men suffer from generalized anxiety, social anxiety, or panic disorder without seeking help due to stigma or minimization (AAMC, 2023).
3. Substance Use and Addiction
Men show higher rates of substance use disorders, which frequently co-occur with mood or anxiety disorders (Möller-Leimkühler, 2023). In many cases, substance use serves as an avoidant coping mechanism that conceals emotional distress.
4. Suicide and Self-Harm
Suicide remains one of the leading causes of death among men. Although fewer men are diagnosed with depression, they die by suicide three to four times more often than women (World Health Organization, 2023). This discrepancy underscores the urgent need for male-sensitive suicide prevention strategies.
Why Is Men’s Mental Health So Overlooked?
The neglect of men’s mental health stems from a complex web of cultural, social, and systemic factors that reinforce silence and underdiagnosis:
- Rigid Masculinity Norms — Deeply ingrained beliefs that “real men don’t cry” or should suppress emotions discourage vulnerability and help-seeking (Mokhwelepa & Sumbane, 2024).
- Stigma and Self-Stigma — Fear of being perceived as weak or unstable prevents many men from acknowledging their struggles or pursuing therapy (Pederson & Vogel, 2021).
- Diagnostic Bias — Mental health professionals may misinterpret or overlook externalized symptoms such as anger, irritability, or risk-taking, which often mask underlying distress (Cochran & Rabinowitz, 2020).
- Limited Emotional Literacy — Many men have not been socialized to recognize or articulate emotions, making it difficult to identify early signs of depression or anxiety (Bonabi et al., 2016).
- Structural Barriers — Long work hours, financial pressures, and a shortage of male-friendly mental health services make access to care especially challenging (Thompson et al., 2024).
- Insufficient Research and Policy Attention — For decades, mental health initiatives have been designed primarily with gender-neutral or female-centered approaches, leaving men’s specific needs underexplored (Seidler et al., 2016).

Early Warning Signs to Watch For
Men often experience and express emotional distress differently than women — not always through visible sadness or crying. Instead, their symptoms can appear as behavioral or physical changes that may go unnoticed until they intensify. Recognizing these early signs is crucial for prevention and timely support (Mahalik et al., 2022; Seidler et al., 2021):
- Persistent irritability, frustration, or anger — Chronic irritability can mask depression or anxiety, especially when emotional expression feels culturally restricted.
- Withdrawal from family, friends, or hobbies — A gradual loss of interest in previously meaningful activities may signal emotional exhaustion or isolation.
- Fatigue or disrupted sleep — Difficulty falling asleep, oversleeping, or constant tiredness often accompany stress-related disorders.
- Increased use of alcohol or drugs — Substance use may become a coping mechanism to manage unexpressed emotions (Oliffe et al., 2020).
- Reckless or risky behavior — Engaging in dangerous activities or taking unnecessary risks can reflect emotional numbness or a need to escape.
- Declining performance at work or school — Difficulty concentrating or maintaining motivation may indicate burnout or depressive symptoms.
- Feelings of hopelessness or emptiness — When combined with emotional withdrawal, these feelings can signal major depression or suicidal ideation.
Recognizing these warning signs — in oneself or in loved ones — is often the first and most powerful step toward healing. Compassionate attention and early intervention can make a significant difference in outcomes (World Health Organization [WHO], 2023).
Suicide Prevention and Early Intervention
Preventing suicide among men requires more than awareness — it demands culturally responsive, evidence-based, and compassionate approaches that acknowledge how men experience and express distress. Research indicates that prevention strategies tailored to men’s realities are significantly more effective than generic interventions (Englar-Carlson & Kiselica, 2013; Seidler et al., 2021).
Key strategies include:
- Encouraging open, stigma-free conversations — Honest dialogue about emotions and mental health helps dismantle the belief that vulnerability equals weakness (Mahalik et al., 2022).
- Promoting access to crisis services and hotlines — Readily available, confidential support lines such as 988 in the U.S. can provide immediate assistance and save lives.
- Ensuring consistent follow-up care — Ongoing professional support after suicidal thoughts or attempts significantly reduces recurrence risk (WHO, 2023).
- Reducing structural and cultural barriers — Making healthcare settings more approachable and male-friendly encourages men to seek help earlier.
- Securing firearms and medications — Safe storage practices in households with at-risk individuals are proven to lower suicide fatalities (Butterworth et al., 2022).
Ultimately, male-sensitive prevention integrates positive masculinity, emphasizing strength through connection, responsibility, and community involvement — not silence.
Empowering men to seek help, connect with peers, and engage in therapy can change outcomes and save lives.
Evidence-Based Treatment and Support
Psychotherapy
Cognitive Behavioral Therapy (CBT), Behavioral Activation, and Motivational Interviewing (MI) have demonstrated high efficacy in treating depression and anxiety among men (Smith et al., 2024). Men often respond best to structured, goal-oriented approaches that emphasize practical outcomes.
Peer and Community Support
Peer groups and male-specific support programs reduce isolation and normalize emotional expression. Initiatives such as HeadsUpGuys and Man Therapy have shown promise in improving help-seeking behaviors among men (Seidler et al., 2016).
Medication and Integrated Care
When clinically indicated, antidepressants or mood stabilizers can complement therapy. Integrated care models — which combine physical and mental health services — help reduce fragmentation and improve outcomes (Thompson et al., 2024).
Telehealth and Digital Tools
Teletherapy and online mental health apps have become key resources for men reluctant to seek in-person treatment. These tools offer privacy and flexibility, reducing barriers to engagement (Smith et al., 2024).
How to Help a Partner, Friend, or Family Member Who Is Struggling
Supporting someone you love through a mental health challenge can feel daunting — especially when that person seems withdrawn, defensive, or unwilling to talk. However, research shows that compassionate connection can significantly reduce emotional isolation and increase the likelihood of seeking professional help (Addis & Mahalik, 2003).
Here’s how to offer meaningful support:
1. Start with Presence, Not Pressure
Simply being there matters. Sit with them, listen, and allow silence. Avoid rushing to “fix” the problem — focus instead on understanding how they feel.
2. Use Nonjudgmental and Validating Language
Avoid minimizing their experiences. Phrases like “I can see this is really hard for you” or “You don’t have to go through this alone” can make a major difference.
3. Recognize Defensive Reactions
Many men feel embarrassed or ashamed about emotional pain. If your loved one reacts with anger, defensiveness, or withdrawal, interpret it as distress — not rejection. Maintain calm empathy and give them space to re-engage.
4. Encourage Professional Support Gently
Offer to help them find a therapist or attend the first session together. Framing therapy as “a step toward feeling better” rather than “a sign of weakness” can reduce resistance.
5. Watch for Red Flags
If they mention hopelessness, self-harm, or feeling like a burden, take it seriously. Encourage immediate professional help or contact crisis services if necessary.
6. Take Care of Yourself, Too
Supporting someone with mental health struggles can be emotionally taxing. Prioritize your own mental wellbeing, and seek support if you need it.
Empathy, patience, and consistent presence are often more powerful than perfect words.
Redefining Strength: Toward a Healthier Masculinity
To foster long-term change, society must move away from outdated ideals of masculinity and redefine strength as the ability to seek support, show emotion, and connect authentically.
- Promote Positive Masculinity: Emphasize traits like integrity, empathy, and courage as compatible with emotional openness (Englar-Carlson & Kiselica, 2013).
- Normalize Emotional Literacy: Teach boys and men to identify and articulate their emotions early.
- Encourage Workplace and Policy Reform: Advocate for mental health days, flexible schedules, and Employee Assistance Programs (EAPs).
- Invest in Research: Expand studies focused on male mental health and male-specific therapeutic approaches.
Every Man Deserves to Heal, Grow, and Be Heard
Men’s mental health challenges are real, and silence only deepens them. Understanding, compassion, and culturally aware care can change outcomes — and save lives.
If you or someone you know is struggling, Sessions Health offers confidential, professional support through therapy, psychiatric evaluation, and personalized treatment plans — in person, online, or hybrid.
Your mental health matters. Healing and hope are possible.